An in-depth analysis of the effectiveness, safety, and indications of "embryo glue"

Click the image to watch the video on YouTube.
EmbryoGlue is not simply glue, but a transfer medium rich in hyaluronic acid that mimics the natural secretions of the uterus to facilitate implantation. According to the Cochrane Review (2020), its use significantly increases the live birth rate (from approximately 33% to 40-44%). While effective, it is particularly recommended for patients over 35 years old, cases of repeated implantation failure (RIF), and fresh embryo transfers.
- 📌 In this article, you will learn:
- What exactly is EmbryoGlue?
- The Mechanism: How does it work? (The bridge analogy)
- Scientific Evidence: What do the numbers say?
- Fresh vs. Frozen Cycle: The important distinction
- Who should use EmbryoGlue?
- Safety and Side Effects
- FAQ: Your frequently asked questions
Introduction
After more than thirty years of clinical practice, one observation constantly recurs: for couples embarking on an IVF journey, the most difficult moment is not the egg retrieval. It’s the waiting. The waiting that follows embryo transfer.
At this stage, everything seems to be in place: the embryo is of good quality, the uterus is receptive, conditions appear ideal. And yet, implantation doesn’t always occur. This element of uncertainty, often experienced as a genuine emotional ordeal, is what we call the “black box” of IVF.
For years, research has been working to better understand and optimize this critical moment: the encounter between the embryo and the endometrium. It is with this goal in mind that EmbryoGlue emerged, a transfer medium enriched with hyaluronic acid. Far from being merely a marketing gimmick, it is based on a clear principle: drawing inspiration from natural mechanisms to provide the embryo with an environment more conducive to implantation.
What Exactly is EmbryoGlue?
Contrary to what its name might suggest, EmbryoGlue is not an artificial “glue” in any way. It is not an adhesive product, but rather a specific culture medium used exclusively at the time of embryo transfer.
This medium is enriched with two essential components, carefully chosen for their biological role:
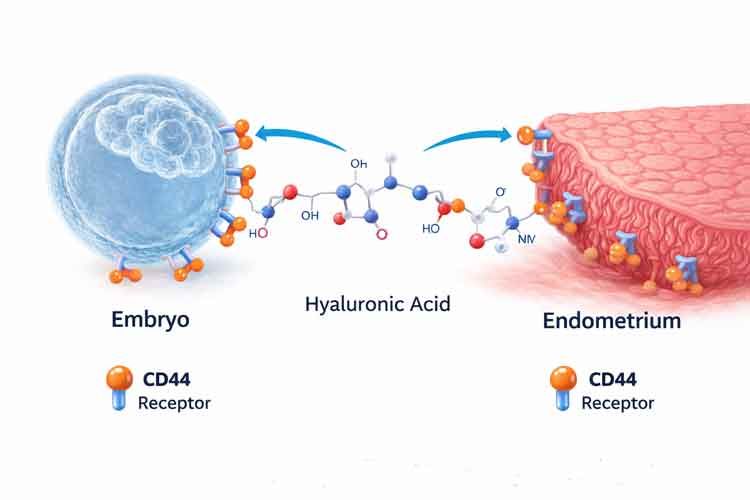
1. Hyaluronic Acid (HA) This molecule is naturally present in the uterus. Its levels increase dramatically at the precise moment when the endometrium becomes receptive, during the famous implantation window. It participates in communication between the embryo and the uterine lining.
2. Recombinant Human Albumin This is a highly purified protein, produced without risk of viral transmission. It helps support embryonic metabolism and stabilize the embryo’s immediate environment.
In a natural cycle, the uterus transforms just before implantation: the medium becomes more viscous, richer in hyaluronic acid, and therefore closer to optimal conditions for the embryo. In contrast, standard culture media are very fluid, comparable to water.
The objective of EmbryoGlue is precisely to reduce this biological gap by more faithfully reproducing the natural uterine environment through increased viscosity and high concentration of hyaluronic acid.
The Mechanism: How Does It Work?
To understand how EmbryoGlue works, I often use a simple analogy with my patients:
- The Bridge and Velcro Analogy: Imagine that the embryo is a boat and the endometrium (the uterine wall) is the dock. For the passenger (pregnancy) to disembark, the boat must be stable.
- Mechanical Effect (Viscosity): EmbryoGlue thickens the water, preventing the boat from drifting too quickly or being expelled by currents (uterine contractions).
- Biological Effect (CD44 Binding): This is the most important. Both the embryo and the uterus have receptors called CD44. Hyaluronic acid acts as a molecular bridge that binds to both sides simultaneously, creating a sort of “biochemical Velcro” that stabilizes the embryo so it can initiate tissue invasion.
Scientific Evidence: What Do the Numbers Say?
The effectiveness of EmbryoGlue has long been debated in scientific literature. However, we now have robust data to clarify this question, particularly thanks to the 2020 Cochrane Review, published by Cochrane and widely recognized as one of the major references in medical evidence.
Here are the key results based on analysis of more than 6,704 patients (Source: Cochrane Database Syst Rev. 2020):
📊 EmbryoGlue Karşılaştırma Tablosu
| Parameter | Standard Medium | With EmbryoGlue | Relative Gain | Significance |
|---|---|---|---|---|
| Live Birth Rate | ~33.0% | ~40.2% | +21% (RR 1.21) | ✅ Proven |
| Clinical Pregnancy | Baseline | Increased | +16% (RR 1.16) | ✅ Proven |
| Miscarriage | Baseline | Slight Decrease | -18% (RR 0.82) | 📉 Possible |
| Multiple Pregnancy | Baseline | Increased* | +45% (RR 1.45) | ⚠️ Caution |
Clinical Note: The observed increase in multiple pregnancies does not mean that EmbryoGlue creates a risk per se. It is simply explained by improved embryo implantation capacity. This is precisely why I very often recommend elective single embryo transfer (eSET) when EmbryoGlue is used, to maximize success rates while limiting obstetric risks.
The NNT (Number Needed to Treat) concept provides a very concrete understanding of these results. The data shows that approximately 14 patients need to be treated with EmbryoGlue to obtain one additional live birth that would not have occurred without its use. In reproductive medicine, this is a particularly significant figure that reflects a real and measurable clinical benefit.
Fresh vs. Frozen Cycle: The Important Distinction
This is where clinical expertise is crucial. The effectiveness of EmbryoGlue varies depending on the type of cycle.
1. Fresh (Stimulated) Cycles
During IVF with fresh transfer, hormone levels are deliberately very high. This hyperstimulation, essential for treatment, can however disrupt the physiological balance of the endometrium. In particular, it can impair its ability to produce sufficient hyaluronic acid at the crucial moment of implantation.
In this specific context, EmbryoGlue acts as a compensatory tool. By locally providing the missing hyaluronic acid, it helps restore a more favorable environment around the embryo. The goal is not to artificially provoke implantation, but rather to get as close as possible to the natural conditions in which it usually occurs.
- Verdict: Strongly recommended, supported by ESHRE guidelines.
2. Frozen Cycles (FET)
In frozen cycles, the hormonal environment is closer to natural. ESHRE (2023) did not recommend systematic use in frozen cycles. However, very recent 2024 studies including nearly 1,300 cycles show that EmbryoGlue significantly improves birth rates (60.6% vs 47.5%) even in frozen cycles, especially in women over 35 years old.
My opinion: In frozen cycles, EmbryoGlue should not be used systematically. Its indication must be thoughtful and personalized. However, the most recent data is clearly encouraging in patients who have already experienced one or more implantation failures, in whom this approach can provide real benefit.
Who Should Use EmbryoGlue?
Although its benefits are well established, EmbryoGlue is by no means a solution to be applied systematically. Its use must remain targeted and thoughtful. In my practice, I recommend it more readily for certain profiles for whom it can provide real added value:
-
Repeated Implantation Failure (RIF) In patients who have experienced at least three transfers of good quality embryos without success, the hypothesis of an embryonic adhesion defect becomes plausible. EmbryoGlue can then help overcome this critical step.
-
Advanced Maternal Age (over 35–38 years) With age, the expression of certain receptors involved in implantation may decrease. The addition of hyaluronic acid aims to partially compensate for this decline and improve the embryo’s reception environment.
-
Unexplained Infertility When all standard parameters are reassuring but pregnancy does not occur, optimizing the embryonic adhesion phase appears as a logical and coherent approach.
-
Technically Difficult Transfers In situations where cervical passage is delicate or manipulations more complex, the viscosity of the medium can play a protective role, limiting mechanical stress on the embryo.
Safety and Side Effects
This is a legitimate question: is it safe for the baby? The scientific answer is reassuring, as emphasized by the British authority HFEA.
-
Congenital Malformations To date, no increased risk of malformations has been demonstrated in children from transfers performed with EmbryoGlue.
-
Newborn Health Available follow-up studies show comparable health at birth, with no significant difference compared to transfers performed with standard media.
-
Origin and Safety of Albumin The albumin used is produced by yeast, with no animal or human origin. This process eliminates any risk of viral transmission and guarantees a high level of biological safety.
FAQ: Your Frequently Asked Questions
1. Does EmbryoGlue increase the risk of identical twins?
EmbryoGlue does not cause embryo division and therefore does not create monozygotic twins. However, when two embryos are transferred, this technique increases the probability that both will implant simultaneously.
This is precisely why we favor, in the vast majority of cases, single embryo transfer (SET) when using EmbryoGlue. This strategy allows us to benefit from improved implantation while limiting the risk of multiple pregnancies, which remain associated with more obstetric complications.
2. How much does this additional treatment cost?
The cost of EmbryoGlue generally remains moderate when placed in the overall context of an IVF cycle. In Europe, it is most often between €200 and €250.
In our practice, we consider it an accessible add-on with a particularly interesting cost-effectiveness ratio, especially for patients for whom improving implantation chances can avoid additional attempts, often much more costly financially and emotionally.
3. Can I use EmbryoGlue for my first IVF?
Yes, it is entirely possible, particularly after age 35, where every detail that can improve implantation deserves consideration. However, in a younger patient with an excellent prognosis and already very favorable conditions, the benefit remains often more modest.
In other words, the value of this approach increases with profile complexity and should always be evaluated with a logic of personalization rather than automation.
4. Does it replace genetic testing (PGT-A)?
No. EmbryoGlue facilitates embryo implantation, but it has no effect on its genetic quality. It therefore cannot correct a chromosomal abnormality.
A genetically abnormal embryo may sometimes implant, but it will most often progress to early miscarriage, with or without EmbryoGlue. This is an essential point to understand.
In this logic, the two approaches are complementary:
- genetic testing aims to select a chromosomally normal embryo,
- EmbryoGlue seeks to optimize the conditions of its implantation.
One does not replace the other; they simply act at two different stages of the process.
5. How does the procedure work for me?
For you, nothing changes. The entire process takes place entirely in the laboratory, without modification to the transfer procedure.
Specifically, the embryologist places the embryo in this specific medium for a period ranging from 10 minutes to a few hours before transfer. This exposure time allows the hyaluronic acid to bind to the embryo’s receptors, to optimize the conditions for implantation.
Conclusion and Next Steps
EmbryoGlue today represents an important advance in our ability to approach natural mechanisms to improve IVF outcomes. Available data shows a documented increase in live birth rates, associated with an excellent safety profile. This is why it is one of the options we take time to discuss when the goal is to optimize your chances, particularly if your journey has already been marked by failures.
But in reproductive medicine, there is no universal solution. Every story is unique. During your next consultation, we will evaluate together whether this approach can truly integrate into your personal situation and become, perhaps, the missing piece in your own path to parenthood.
⚖️ Legal Disclaimer
Publication Date: January 30, 2026
This article was written by Dr. Senai Aksoy for exclusively informational purposes and cannot substitute for personalized medical advice. Every patient is unique, and the results of in vitro fertilization treatments can vary based on numerous individual factors.
For any questions regarding your personal situation, your health, or your treatment options, it is essential to consult your specialist physician.
© Dr. Senai Aksoy – All rights reserved.
The content has been created by Dr. Senai Aksoy and medically approved.

