Screening Hysteroscopy Before IVF. When Is It Really Necessary?

Recent data, especially from the ESHRE 2023 meeting, shows that doing a hysteroscopy before the very first IVF try doesn’t really improve the chances of a live birth. So, if you don’t have any specific risk factors, this test probably won’t make things better.
But, things change if you’ve had trouble with embryo transfers not working. If you’ve had two to four tries that didn’t work out, then a hysteroscopy might be a good idea. It can spot (and sometimes fix) problems in your uterus that didn’t show up on an ultrasound. These issues are found in about 25% of these cases, which could explain why things didn’t work before.
Click on the image to watch the video on YouTube.
📌 What Will You Discover in This Article?
- What is screening hysteroscopy?
- Hysteroscopy before the first IVF: what do recent studies say?
- Hysteroscopy and repeated implantation failure: a proven benefit?
- What abnormalities can hysteroscopy reveal?
- Hysteroscopy vs Ultrasound: what is the difference?
- How is a diagnostic hysteroscopy performed?
- When should hysteroscopy be recommended before IVF?
- FAQ: Your most frequently asked questions
What Is Screening Hysteroscopy?
Screening hysteroscopy, also known as diagnostic hysteroscopy, is an examination that allows direct exploration of the inside of the uterus and the cervical canal using a very thin instrument called a hysteroscope. Unlike transvaginal ultrasound or hysterosalpingography, which provide indirect imaging, this technique offers direct, real-time visualization of the endometrium.
In my 30+ years of practice, I’ve seen how helpful hysteroscopy is for spotting small problems that don’t always show up on regular scans. Think of it like a tiny camera that goes inside your uterus. If ultrasound is like looking at a house from the street, hysteroscopy lets you check out every room inside. Often, the important clues for understanding what’s going on are found in these little details.
The Goals of Hysteroscopy Before IVF
Hysteroscopy before IVF can notably:
- Find any endometrial polyps that could mess with the embryo sticking around.
- Spot submucous fibroids that change the shape of the uterus and stop implantation.
- See uterine synechiae (adhesions), which usually don’t show up on regular ultrasounds.
- Point to chronic endometritis, a tricky inflammation of the endometrium that can cause issues.
- Check how the uterine cavity looks, mainly if there might be something wrong from birth.
💡 Important: We know hysteroscopy can find problems. The real question is: when does it actually help you get pregnant?
Hysteroscopy Before the First IVF: What Do Recent Studies Say?
The Cochrane Review and Multicenter Studies
A Cochrane review from 2019 initially suggested a possible benefit of hysteroscopy before IVF, with a relative risk of 1.26 for live births. However, this analysis had significant limitations:
There are a few things that might explain why the results sometimes don’t match up.
First off, when you look at all the studies together, there’s a lot of difference between them. This means the results change quite a bit from one study to the next, which makes it harder to draw solid conclusions.
Also, the people in the studies aren’t all the same. Some studies have people doing IVF for the first time, while others only look at people who’ve had it fail before. Mixing these groups can make it hard to see if anything is really working.
Lastly, the way the studies were done wasn’t always the best. They had unlike rules for who could join, followed different steps, and might have had some biases. All of this makes it tricky to figure out what’s really going on.
The Decisive Point
Here’s something really interesting: When researchers only looked at studies that followed really careful methods, any possible advantage of hysteroscopy went away.
The risk became neutral,meaning that in the best studies, hysteroscopy didn’t really change the results, especially when it came to things like getting pregnant or having a baby.
The inSIGHT and TROPHY Studies: The Definitive Answer
Two large multicenter randomized studies settled the question:
inSIGHT Study (Netherlands, 2016)
We did a study with 750 women who were about to try IVF for the first time. Before starting, they all had a normal uterine ultrasound, meaning there were no visible problems inside the uterus.
We split the women into two groups:
- 373 had a hysteroscopy before IVF
- 377 didn’t have any other tests
The results were pretty straightforward: the live birth rates were about the same in both groups.
The stats showed a relative risk of 1.06, with a confidence interval of 0.93 to 1.20. Basically, if you have a normal ultrasound, getting a hysteroscopy before your first IVF doesn’t really make a difference in whether you’ll have a baby.
This backs up what other studies have found: if there’s no reason to think there’s something wrong, checking the uterus beforehand doesn’t seem to help with live birth rates.
TROPHY Study (European Multicenter, 2016)
A study looked at 702 women who had two to four failed embryo transfers to see if extra testing would help.
At first, all the women had ultrasounds that looked okay, meaning there were no obvious problems.
But when they did more tests, they found issues in 24% of the women. That might sound like a lot, but only 4% of those problems could actually be fixed.
Here’s the most important thing: Even after finding and fixing those problems, the number of live births didn’t really increase.
Basically, even though they found some things wrong after a few failed transfers, fixing them didn’t help the women get pregnant in this study.
Furthermore, the study by Ben Abid and colleagues (2021) confirmed these results: 23.9% pregnancy rate with hysteroscopy vs 19.3% without hysteroscopy (p = 0.607).
Current ESHRE Recommendation (2023)
According to the ESHRE recommendations on repeated implantation failure, screening hysteroscopy is currently not recommended for routine clinical use before the first IVF.
| Situation | Recommendation | Level of Evidence |
|---|---|---|
| Before 1st IVF with normal ultrasound | Not recommended | Grade A (strong) |
| Before 1st IVF with ultrasound abnormality | Recommended | Grade B |
| After 2-4 IVF failures | May be considered | Grade C |
Hysteroscopy and Repeated Implantation Failure: A Proven Benefit?
But things change when we talk about repeated implantation failure (RIF).
RIF usually means you don’t get pregnant after three transfers of good embryos, or after transferring at least eight embryos overall.
Basically, it’s not just a one-time thing; it keeps happening even when things look good. So, in this case, the way doctors test and treat it might be different because the reasons could be more specific, and it needs a closer look.
Contradictory Data
A meta-analysis by Cao and colleagues (2018) reported a relative risk of 1.29 (95% CI: 1.03-1.62) in favor of hysteroscopy in patients with repeated failures. However, this analysis included observational studies and not exclusively randomized trials.
Paradoxically, the largest randomized study included (TROPHY study with 702 patients) found no significant difference.
My 30 Years of Clinical Experience
I’ve noticed that when I do hysteroscopies on women after they’ve had trouble with implantation, I find something unusual in about 25% of them.
That might sound like a lot, but usually, it’s something small. Also, fixing it doesn’t always mean they’ll have better luck getting pregnant.
Most Frequently Observed Abnormalities
So, looking back at the data, we often see a few things pop up:
- Chronic endometritis shows up in about 15-25% of cases.
- Endometrial polyps are in 10-15% of cases.
- Minimal synechiae appear in 5-10% of cases.
- An abnormal looking lining is seen in 8-12% of cases
But, it’s important to know that not all of these things affect the outlook in the same way.
What Is the Real Benefit of Treatment?
How much it helps really depends on what kind of problem we find:
- Big help: If there are polyps bigger than 10 mm or fibroids under the lining. Taking care of these can really make the uterus a better place.
- Some help: If it’s chronic endometritis (long-term inflammation of the uterine lining), the right antibiotics might make it easier for an embryo to implant, but it’s not a sure thing.
- Maybe not much help: For small problems with the uterine lining, fixing them might not change how things turn out.
🔬 My Clinical Perspective
So, even though it might not work the first time, hysteroscopy is generally better at helping to figure out what’s going on and what to do next, instead of being a quick fix for getting pregnant.
The best thing about it is that it helps doctors check for any rare problems that can be fixed. This can be really useful because it assures you that the doctors have checked everything carefully.
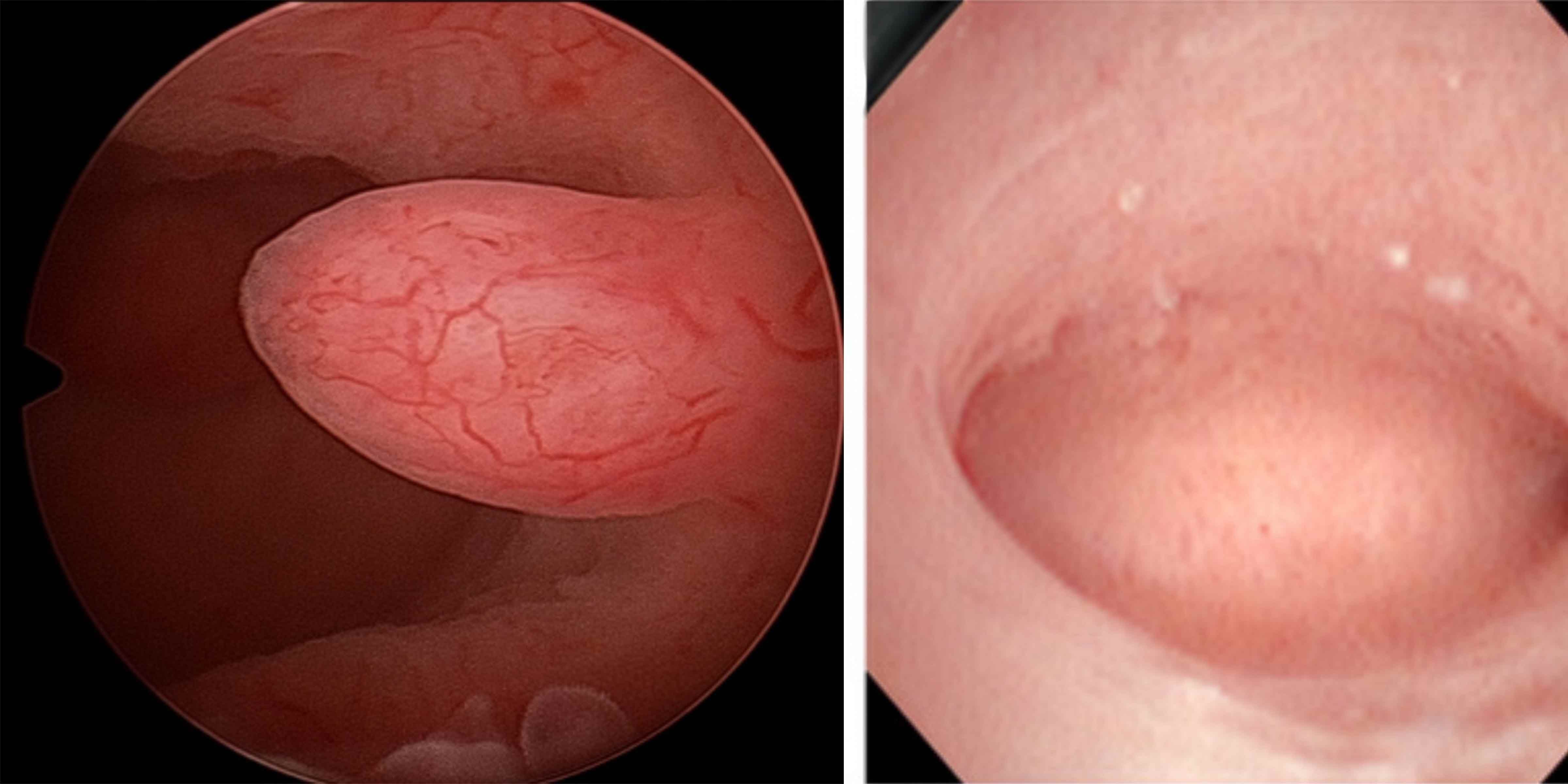
What Abnormalities Can Hysteroscopy Reveal?
Classification of Uterine Abnormalities
| Type of Abnormality | Frequency in RIF | Impact on IVF | Treatment |
|---|---|---|---|
| Endometrial polyps | 10-15% | ⚠️ Moderate to high (especially if > 10 mm) | Hysteroscopic polypectomy |
| Submucous fibroids | 3-5% | ⚠️⚠️ High (cavity distortion) | Hysteroscopic myomectomy |
| Uterine synechiae | 5-10% | ⚠️⚠️ High (reduced implantation surface) | Hysteroscopic adhesiolysis |
| Chronic endometritis | 15-25% | ⚠️ Moderate | Antibiotics (doxycycline) |
| Partial uterine septum | 1-3% | ⚠️⚠️ High | Hysteroscopic septoplasty |
| Abnormal mucosal appearance | 8-12% | ? Uncertain | No specific treatment |
Focus: Chronic Endometritis
Chronic Endometritis: An Often Silent Cause
Chronic endometritis is when the lining of your uterus gets inflamed, but it’s sneaky because it usually doesn’t cause many symptoms. Sometimes, you might not even know you have it.
If you look at the tissue under a microscope, you’ll see plasma cells where they shouldn’t be. That’s a sign that there’s some inflammation going on for a while.
How Common Is It?
The rate of this issue changes a lot depending on who you’re looking at:
- For people who have trouble getting pregnant in general: 10 to 15%
- For people who have tried IVF many times without success: 42 to 44%
This big difference makes you think it might cause problems with the fertilized egg attaching to the uterus, but whether it actually causes the problem is still up for debate.
How Is It Diagnosed?
To figure out what’s going on, doctors use specific tests:
- Endometrial biopsy: They take a sample of your uterine lining and look at it under a microscope. This is key to seeing if plasma cells are present.
- CD138 immunostaining: This test helps spot those inflammatory cells I mentioned.
- During a hysteroscopy (where they look inside your uterus with a camera), they might see things like redness, small red spots, or a slightly bleeding surface.
Keep in mind that just looking at it isn’t enough to know for sure. The biopsy is still the best way to confirm a diagnosis.
What Is the Treatment?
The usual treatment involves antibiotics, most often:
- Doxycycline 100 mg, twice a day, for 2 weeks.
After you finish the antibiotics, your doctor might want to do another check (either with a hysteroscopy or a biopsy, depending on your situation) to make sure the inflammation is gone.
The info we have is still coming together, but first studies show that some patients have a better chance of getting pregnant after the treatment, which is good news.
Hysteroscopy vs Ultrasound: What Is the Difference?
Comparative Table of Examinations
| Criteria | Transvaginal Ultrasound | Hysterosalpingography (HSG) | Diagnostic Hysteroscopy |
|---|---|---|---|
| Principle | Ultrasound waves through the wall | X-ray with contrast agent | Direct visualization by camera |
| Sensitivity for abnormalities | 35% | 40% | 100% (by definition) |
| Specificity | 82% | 86% | 100% (reference examination) |
| Tubal patency | ❌ No | ✅ Yes | ❌ No (except visible hydrosalpinx) |
| Pain | None | Moderate (cramps) | Mild to moderate |
| Anesthesia | No | No | No (office hysteroscopy) |
| Duration | 5-10 min | 15-20 min | 5-10 min |
| Approximate cost | $50-100 | $150-250 | $200-400 |
The Complementarity of Examinations
In my practice, I favor a progressive and reasoned approach. The goal is not to multiply examinations, but to use them at the right time.
1️⃣ Transvaginal Ultrasound: The Foundation
A transvaginal ultrasound is still the best first step. It’s a normal, simple test that gives us a ton of info about your uterus and endometrium.
Most of the time, it helps us spot things that are clearly not right and tells us what other tests we might need.
2️⃣ Hysteroscopy: Targeted, Not Automatic
I usually suggest a hysteroscopy if:
- An ultrasound shows something unusual.
- You’ve had trouble getting pregnant after multiple IVF attempts.
It’s not something I do for everyone, but it is helpful when I need a closer look.
3️⃣ Hysterosalpingography: A Different Purpose
Hysterosalpingography has a specific job. It mainly checks if your fallopian tubes are open. While it gives a quick look at your uterus, it’s not really meant for a detailed inspection.
💭 A Metaphor for Better Understanding
I usually put it this way:
Think of ultrasound as looking at your house from the curb. Then, hysteroscopy is like walking through each room with a flashlight.
You’re bound to see more stuff – even little things you couldn’t spot from outside.
But here’s the thing: Do you really need to scout every corner of a house to know if you can live there?
That’s where things get tricky in fertility treatment. It’s about figuring out how much looking around is enough to actually help.
Combined Sensitivity
A study in Tunisia in 2012 looked at how well ultrasound and HSG, used together, could find problems, using hysteroscopy as the standard test.
If at least one of the ultrasound or HSG tests came back with an abnormal result, the combined method was able to correctly identify about 73% of the issues that hysteroscopy could see.
Basically, this approach catches almost three out of four problems that a hysteroscopy would find.
What Does This Number Mean in Practice?
So, about 27% of issues found during hysteroscopy aren’t spotted by ultrasound and HSG together.
These often include:
- long-term womb lining inflammation
- slight scarring
- tiny growths
Usually, they’re not big problems, but more like small things that you can only see when you look directly inside the womb.
This then begs the question: do these overlooked issues actually affect whether someone can have a baby?
That’s where the experts still disagree.
How Is a Diagnostic Hysteroscopy Performed?
Before the Examination
When Should Hysteroscopy Be Performed?
The best time to do it is usually between day 5 and day 14 of your cycle, so during the early follicular phase.
Why this time frame?
- Your period just ended, making it way easier to see things inside your uterus.
- The endometrium is still thin, allowing for easier looking around. You haven’t ovulated yet, so there’s no chance of messing with an early pregnancy.
This timeframe gives the best situation for getting clear results and doing the procedure well.
Is Any Special Preparation Required?
Usually, you don’t have to do anything special to get ready.
For a diagnostic hysteroscopy done through vaginoscopy:
- No need for general anesthesia.
- You don’t usually need antibiotics beforehand, following the French National College of Gynecologists and Obstetricians’ advice (CNGOF, grade B).
- If you think you need it, you can just take a simple pain reliever like paracetamol (acetaminophen) about an hour before.
The exam is usually quick, not too bad, and can be done right in the office.
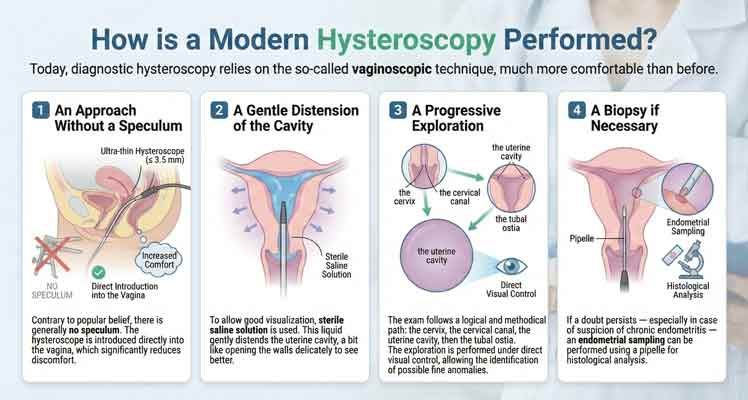
During the Examination (Vaginoscopic Technique)
How Is a Modern Hysteroscopy Performed?
These days, when doctors use a hysteroscope to look inside the uterus, they usually use a method called the vaginoscopic technique. It’s a lot easier on the patient than older ways of doing it.
1️⃣ A Speculum-Free Approach
Actually, you usually don’t need a speculum. The hysteroscope, which is this really thin tool (like, 3.5 mm or less), goes right into the vagina, so it’s not as uncomfortable.
2️⃣ Gentle Distension of the Cavity
To get a clear view, we use sterile saline solution. This fluid carefully expands the uterus, kind of like opening it up so we can see things better.
3️⃣ A Progressive Exploration
The exam goes step-by-step:
- First, the cervix.
- Then, the cervical canal.
- After that, the uterine cavity.
- Finally, the tubal ostia (that’s where the fallopian tubes open up). We do this while looking directly, so we can spot even small problems.
4️⃣ A Biopsy If Necessary
If doubt persists — particularly in cases of suspected chronic endometritis — an endometrial sample can be taken using a pipelle for histological analysis.
⏱️ How Long Does the Examination Take?
The whole thing usually takes about 5 to 15 minutes.
Most of the time, it’s done right in the office, so you don’t have to go to the hospital or be put to sleep.
Sensations and Pain
A British study from 2021 by Mahmud and his team looked at how much pain women feel during hysteroscopies, and the results are pretty interesting.
The study found that 87% of women said they felt some pain during the procedure. Of those women:
- 41% said the pain was more than just slightly painful.
- On a scale of 1 to 10, the average pain level was 4.69.
These numbers remind us that even though it’s a diagnostic procedure, hysteroscopy can be painful.
Pain That Varies Greatly from Patient to Patient
From what I’ve seen, everyone experiences this differently. Some people feel a little discomfort for a short time, but others say it’s much more intense.
A few things can make it feel worse:
- Never having given birth
- A narrow cervix
- Feeling really anxious beforehand
On the bright side, these things can help:
- Using a thin hysteroscope
- Having an experienced doctor
- Expanding the cavity slowly and carefully
Basically, how it’s done and the setting make a big difference.
💡 Practical Tip
Here’s a tip that’s simple but works well:
Try slow, deep breathing during the exam.
This kind of breathing can help your pelvic floor relax and make you feel less pain. It’s a small thing that can really help!
After the Examination
What Are the Usual After-Effects of Hysteroscopy?
Most people experience only minor and temporary symptoms after the procedure.
Here’s what you might expect:
- Light spotting for a day or two: This is normal and usually not much.
- Mild cramps: They might feel like period cramps and should only last a few hours.
- Resume normal activities right away: You can usually go back to work and your regular routine immediately.
These symptoms are normal and should go away on their own.
What About Complications?
These are still pretty rare, happening less than 0.5% of the time.
The most reported problems are:
- A hole in the uterus
- An infection (endometritis)
- A vasovagal reaction, which can make someone feel faint for a short time
It’s good to remember that these things don’t happen often, especially if the exam is done right.
When Should Hysteroscopy Be Recommended Before IVF?
Clinical Decision Tree
Here is my personalized approach based on 30 years of experience and ESHRE 2023 recommendations:
✅ Hysteroscopy RECOMMENDED
| Clinical Situation | Indication | Expected Benefit |
|---|---|---|
| Suspicious ultrasound abnormality | Polyp, fibroid, abnormal endometrial thickness | High: diagnosis and treatment |
| Abnormal ultrasound or HSG | Cavity distortion, suspicious image | High: confirmation and treatment |
| ≥ 3 failed transfers of good-quality embryos | Search for subtle abnormality | Moderate: 24% abnormalities detected |
| History of uterine surgery | Cesarean section, myomectomy, curettage | Moderate: risk of synechiae |
| Intermenstrual bleeding | Spotting, metrorrhagia | High: polyps are common |
⚠️ Hysteroscopy TO BE DISCUSSED
| Clinical Situation | Indication | Expected Benefit |
|---|---|---|
| 1-2 IVF failures with good-quality embryos | Comprehensive workup | Low: little impact on prognosis |
| Age > 38 before first IVF | Cavity assessment | Low: age does not increase cavity abnormalities |
| Patient request after normal workup | Reassurance | Psychological: relief of having checked everything |
❌ Hysteroscopy NOT RECOMMENDED
| Clinical Situation | Reason |
|---|---|
| Before 1st IVF with normal ultrasound | No demonstrated benefit (inSIGHT, TROPHY studies) |
| Routinely in the infertility workup | Not cost-effective |
| After 1 single IVF failure | Too early, other causes to explore first |
My Personalized Approach
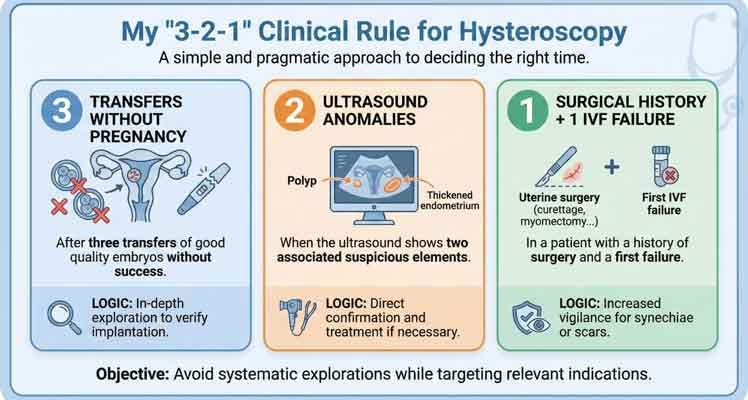
My “3-2-1” Clinical Rule
I use a simple 3-2-1 rule to decide when to suggest a hysteroscopy.
It helps me avoid doing unnecessary tests but still catch things when they’re important.
🔹 3 Transfers Without Pregnancy
If you’ve had three good embryo transfers and still aren’t pregnant, I suggest getting a hysteroscopy.
At this point, it makes sense to look closely and make sure there isn’t anything inside your uterus that’s stopping the embryos from implanting.
🔹 2 Associated Ultrasound Abnormalities
If an ultrasound spots two things that look suspicious, like a polyp along with a thickened endometrium, then a hysteroscopy is a good idea.
The point here isn’t just to look around, but to confirm what the ultrasound saw and deal with it if needed.
🔹 1 Surgical History + 1 IVF Failure
If a patient has had surgery on their uterus before—like a curettage, myomectomy, or a tough C-section—and their first IVF didn’t work, I think about doing a hysteroscopy.
We need to be extra careful because there’s a risk of synechiae or other scarring problems.
A Personalized Rather Than Routine Approach
With this plan, I can focus on patients who really need the help, and not do extra tests on people who are probably fine based on their ultrasound and situation.
In fertility treatments, it’s a constant balancing act: do enough investigation, but not too much treatment.
Can Hysteroscopy Improve Implantation? The “Endometrial Injury” Debate
The Theory of Mechanical Alteration
Some older studies had a cool idea: hysteroscopy might help with implantation, even if everything looks normal.
The thought is that it’s like giving the endometrium a little nudge, what they call endometrial injury, to get things going.
What Is the Biological Hypothesis?
Here’s the main idea:
Making a small change to the lining of the uterus could cause a short-term inflammation in that area.
This inflammation could then cause:
- The release of cytokines, interleukins, and growth factors
- The secretion of pro-implantation proteins such as MUC1, APOD, or PLA2
- A change in the uterus that might make it easier for an embryo to implant
Basically, this small change could signal the body to prep the uterus for pregnancy.
Keep in mind that while this idea makes sense biologically, newer studies have taken a second look and found more complex results.
What Do Recent Data Show?
Okay, so big, well-done studies have given us a straight answer.
The inSIGHT, TROPHY, and Ben Abid (2021) studies all showed there’s really no built-in advantage to getting a normal hysteroscopy.
Basically, even if the exam looks good and there’s been some minor mechanical trauma, pregnancy rates don’t really get better.
An Appealing Theory… But a Fragile One
Looking back, the idea of controlled trauma was mainly based on:
- small studies
- studies where people weren’t randomly chosen
- not enough people in the studies to say for sure
Big trials with many centers and better designs have usually found that a regular diagnostic hysteroscopy by itself doesn’t make implantation more likely.
What About the “Endometrial Injury” Concept?
Okay, so the discussion isn’t really over, but it’s mostly about different methods, like:
- endometrial biopsy using a pipelle
- endometrial scratching
These procedures aren’t the same as a basic diagnostic hysteroscopy. Because of this, you can’t just apply the same biological reasons and patient info from one to the other.
In Summary
Turns out, the idea that a regular hysteroscopy can boost implantation on its own isn’t really backed up by solid proof.
This finding supports taking a careful approach: hysteroscopy is good for figuring out what’s going on, but don’t count on it to be a treatment by itself.
FAQ: Your Most Frequently Asked Questions
1. Is hysteroscopy before IVF mandatory?
No, hysteroscopy is not mandatory before IVF. According to ESHRE 2023 recommendations, it is not indicated as routine practice before the first attempt if your ultrasound is normal. It becomes relevant after several failed embryo transfers or in the presence of ultrasound abnormalities.
2. Does hysteroscopy increase my chances of IVF success?
Not before the first IVF with a normal ultrasound. High-quality multicenter studies (inSIGHT with 750 patients, TROPHY with 702 patients) demonstrated that there is no difference in live birth rates between women who had or did not have a screening hysteroscopy.
However, if hysteroscopy detects and treats a real abnormality (polyp, fibroid, synechiae), then yes, treating that abnormality can improve your chances.
3. After how many IVF failures should I have a hysteroscopy?
The recommendation is to consider hysteroscopy after 2 to 4 failed transfers of good-quality embryos, especially if your initial ultrasound was normal. At this stage, hysteroscopy reveals abnormalities in approximately 24% of cases (TROPHY study), of which 4% are directly treatable.
In my clinic, I generally apply the rule of 3 failed transfers without pregnancy with good-morphology embryos as the threshold for recommending this examination.
4. Is hysteroscopy painful?
Every woman’s experience with pain is different. Around 87% of women feel some discomfort during the exam, rating the pain at about 4.7 out of 10. Some just feel a little pressure, while others have stronger cramps, like period pain.
What affects the pain level:
- The size of the hysteroscope (smaller is better, aim for under 3.5 mm)
- How experienced the doctor is
- How anxious you are
- If you’ve had a baby before (it tends to be less painful for moms)
Quick tip: Taking a regular painkiller like paracetamol an hour before can help ease the discomfort.
5. Hysteroscopy or ultrasound before IVF: which should I choose?
A transvaginal ultrasound is usually the first test done when starting IVF. It’s:
- Not invasive
- Doesn’t hurt
- Doesn’t cost too much
- Good at finding big problems
A hysteroscopy is usually the next test , and it is only done if:
- The ultrasound finds something wrong
- IVF has failed many times
- There are signs of a problem (like bleeding)
You don’t have to pick one. Your doctor will advise hysteroscopy if needed after checking your ultrasound results.
6. What abnormalities can hysteroscopy detect that ultrasound cannot?
Hysteroscopy can show things like:
- Long-term endometritis (inflammation): You can’t see it on an ultrasound.
- Tiny polyps (under 5 mm): Ultrasounds sometimes miss these.
- Slight synechiae (minor adhesions): It’s hard to spot these without looking directly.
- Strange-looking mucosa: Areas that are pale, bleeding, or have lots of blood vessels.
- Tubal openings (how open they are near the start).
About 27% of issues found with hysteroscopy don’t show up on ultrasound and hysterosalpingography together.
7. Should I have a hysteroscopy before my first IVF?
No, you don’t need a routine hysteroscopy before your first IVF if your ultrasound looks good. Solid research says it doesn’t help your chances of success.
But, I would advise it beforehand if:
- Your ultrasound shows something unusual like a polyp, fibroid, or an oddly shaped cavity.
- You’ve had unusual bleeding, like spotting between periods or heavy bleeding.
- You’ve had surgery on your uterus before, such as a C-section, D&C, or myomectomy.
- An HSG (hysterosalpingography) showed that your uterine cavity is distorted.
9. What are the risks of diagnostic hysteroscopy?
Diagnostic hysteroscopy (vaginoscopy) is generally a really safe exam. Problems don’t happen often (less than 0.5% of the time).
Minor issues:
- Some light bleeding (totally normal for a day or two)
- Cramps that aren’t too bad (they should only last a few hours)
- Feeling faint (this doesn’t happen much)
Major issues (really rare):
- A hole being poked in the uterus: less than 0.1% of the time
- Infection of the uterine lining (endometritis): less than 0.3% of the time
- Heavy bleeding: less than 0.1% of the time
A review of studies that included 1,872 patients found that in three of those studies, there were no problems at all. In the fourth study, only one person got endometritis.
10. Can I skip hysteroscopy and go straight to IVF?
Yep, sounds good! If your transvaginal ultrasound looks normal and it’s your first time with IVF, you can go right ahead with the treatment. You don’t need a hysteroscopy as a standard checkup, that’s what’s usually advised.
But, I would suggest a hysteroscopy if:
- You’ve tried IVF 2-3 times already and it hasn’t worked, even with good embryos.
- The ultrasound showed something unusual.
- You’re having problems like irregular bleeding.
The main thing is that you and your doctor talk it over together and decide what’s best for you, based on your situation.
Alternatives to Hysteroscopy
Sonohysterography (Saline Infusion Sonography)
Sonohysterography is basically a vaginal ultrasound that’s done after they put some saline solution into your uterus. The fluid helps to stretch things out so the doctor can see any issues more clearly.
What’s good about it:
- It’s not as invasive as a hysteroscopy.
- It usually doesn’t hurt as much.
- It’s pretty good at spotting polyps and fibroids (over 90% accuracy).
What’s not so good:
- They can’t take a biopsy during the procedure.
- It won’t pick up on ongoing endometritis.
- It’s not the best at finding very small synechiae.
My take: If you’re nervous about getting a hysteroscopy, sonohysterography is a really good middle-ground option compared to a regular ultrasound.
Pelvic MRI
MRI gives us a really clear look at the uterus and surrounding areas.
Good Points:
- It doesn’t involve any cutting or poking.
- It’s great for checking out fibroids (where they are, how big, and how many).
- It can spot adenomyosis.
Not-So-Good Points:
- It can be pricey.
- It’s not good at finding small polyps or endometritis.
- We can’t do any treatment during the scan.
When I use it: If I think someone has a lot of fibroids or adenomyosis and we’re thinking about surgery.
My Holistic Approach After 30 Years of Practice
Beyond the simple question of “hysteroscopy yes or no,” I believe in a personalized and progressive approach:
Step 1: The Baseline Workup (All Patients)
- Quality transvaginal ultrasound
- Complete hormonal panel (AMH, FSH, LH, TSH)
- Partner’s semen analysis
- Hysterosalpingography (tubal patency)
Step 2: The First IVF Attempt
If the workup is normal → IVF attempt without hysteroscopy
Why? Because scientific data show that routine hysteroscopy does not improve your chances. Let’s start with IVF itself.
Step 3: After 1-2 Failures
Thinking it Through:
- What’s the embryo quality like?
- How are the ovaries responding?
- What’s the best way to transfer the embryo?
Hysteroscopy might be a good idea if:
- The embryos look great, but nothing’s implanting.
- There might be an issue with the uterus.
Step 4: After ≥ 3 Failures
Hysteroscopy systematically recommended as part of the repeated implantation failure workup, accompanied by:
- Immunological workup: search for autoantibodies
- Thrombophilia screening: risk of placental microthrombi
- Embryo genetic analysis (PGT-A): aneuploidies
💡 Philosophy of care: Each patient is unique. Statistics guide, but it is your personal history — your symptoms, your results, your expectations — that shapes my recommendations.
Conclusion: An Informed and Personalized Decision
Screening hysteroscopy before IVF is an excellent diagnostic tool, but recent scientific data teach us the importance of not performing it routinely.
What We Know with Certainty
✍️ Summary Conclusion
After analyzing the scientific data and clinical experience, several key points emerge.
🔎 Before a First IVF
Routine hysteroscopy in patients with a normal ultrasound does not improve live birth rates.
The level of evidence is high (grade A). In this context, it should not be offered routinely.
🔁 After Repeated Failures
About 24% of women who have trouble getting pregnant after multiple IVF attempts have uterine issues that can be seen with a hysteroscopy.
Whether or not treating these problems actually helps is still up for debate. The evidence is okay, but not great (grade B-C).
🎯 When a Significant Abnormality Is Identified
But, if the exam finds something obviously wrong—like a polyp bigger than 10 mm, a submucous fibroid, or intrauterine synechiae—and it gets fixed, then there’s a clear and proven health benefit.
When used in these specific cases, hysteroscopy really does what it’s supposed to do, both for finding the problem and fixing it.
🛡️ A Generally Safe Examination
Finally, it is important to remember that diagnostic hysteroscopy is a safe examination, with a very low complication rate (less than 0.5%).
🎯 Key Message
Hysteroscopy isn’t some magical fix, but it’s definitely not worthless either.
It’s helpful when used for the right reason, as part of a plan that fits you.
Don’t just do it automatically. Don’t ignore it when it could help. Do it when it makes sense for you.
✍️ The Real Questions That Remain Open
❓ What Is the Optimal Time to Recommend Hysteroscopy After Failures?
So, how many failed transfers should you have before considering other options? Two, three, or even four?
Well, there’s no easy answer.
Research shows that not much can be learned from testing before three transfers of good embryos. But after three failed attempts, it makes sense to start looking into specific causes.
Really, the call depends on a few things:
- How good were the embryos?
- How old is the patient?
- What’s the history of the uterus?
- What do the ultrasounds show?
Basically, it is not just about the number of tries, but the whole picture.
❓ Do All Detected Abnormalities Deserve Treatment?
This is probably one of the most delicate points.
Some lesions have a clearly demonstrated impact:
- large polyps
- submucous fibroids
- significant synechiae
Their treatment objectively improves the uterine environment.
On the other hand, for minor abnormalities — small polyps, slightly irregular mucosa, filiform synechiae — the line is blurrier.
Are these true causes of failure… or simply anatomical variations with no clinical consequence?
The risk exists of over-interpreting subtle images and treating “false positives” that would probably not have changed the outcome.
❓ Chronic Endometritis: A Real Cause or Just a Marker?
People are still arguing about this question.
It’s interesting that it shows up more often in patients who have repeatedly failed. This makes you think there might be a link. But just because two things are related doesn’t mean one causes the other.
Three hypotheses coexist:
- Chronic endometritis is a direct cause of impaired receptivity.
- It is a contributing factor, among others.
- It constitutes an epiphenomenon, reflecting an inflammatory state or an unfavorable reproductive context.
Early data on antibiotic therapy are encouraging, but they do not yet allow the assertion of a universal benefit.
🎯 In Reality…
These three questions show that deciding to do a hysteroscopy should not be automatic.
It should be a personal decision that considers:
- How likely you are to find something important
- How much the treatment could help
- How hard it is, both mentally and physically, if it doesn’t work the first time
In reproductive medicine, nuance is often more important than a definitive answer.
✍️ Message to Patients
If you are undergoing IVF or facing implantation failures, here is what I want you to remember.
1️⃣ Don’t Feel Obligated
If your ultrasound is normal, there is no urgency or obligation to have a hysteroscopy before a first IVF. Scientific data are reassuring: it does not improve birth rates in this context.
2️⃣ Trust the Progressive Process
Reproductive medicine works in stages. Starting IVF, analyzing results, then adjusting the strategy if necessary is often the most reasonable approach.
Not everything needs to be investigated upfront.
3️⃣ After 2 to 3 Failures, the Thinking Changes
However, after two or three unsuccessful transfers, hysteroscopy becomes a relevant part of the implantation failure workup.
At this stage, it is logical to verify that no subtle abnormality has been overlooked.
4️⃣ If There Is an Abnormality on Ultrasound
If an abnormality is suspected from the start — polyp, atypical endometrium, questionable image — then hysteroscopy is recommended, including before a first IVF.
In this case, it is no longer exploratory, but targeted.
5️⃣ The Decision Must Be Shared
Every journey is unique. Your age, your history, your tolerance for uncertainty, your need to explore “everything right away” or conversely to proceed step by step… all of this matters.
The best decision is one that is discussed and understood, not imposed.
🌿 In Summary
As I often tell my patients:
“Hysteroscopy is neither a miracle nor a mandatory step. It is a valuable tool, to be used at the right time, for the right reasons.”
Legal Notice
Publication Date: February 8, 2026
This article was written by Dr. Senai Aksoy for informational purposes. Each patient is unique. IVF outcomes vary depending on many factors. Always consult a specialist regarding your personal situation.
© Assoc. Prof. Dr. Senai Aksoy - All rights reserved.
The content has been created by Dr. Senai Aksoy and medically approved.