The Role of Hysteroscopy in Improving Fertility. A Comprehensive Overview
The Role of Hysteroscopy in Improving Fertility: A Comprehensive Overview
Introduction
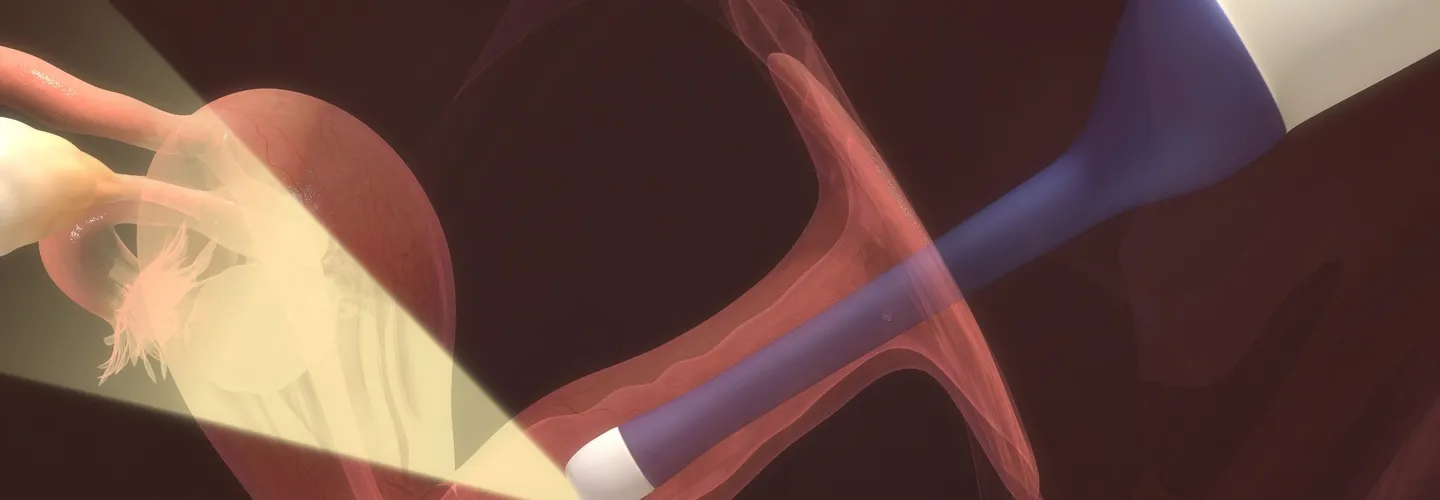
Hysteroscopy is a minimally invasive procedure that allows direct visualization of the uterine cavity. It has become a cornerstone in the diagnosis and treatment of intrauterine pathologies often associated with infertility. This review evaluates the effectiveness of hysteroscopy in improving fertility based on the current medical literature.
Understanding Hysteroscopy
Hysteroscopy involves inserting a hysteroscope—a thin, lighted tube—through the cervix and into the uterus. This procedure can be diagnostic, providing detailed images of the uterine cavity, or surgical, allowing therapeutic procedures to be performed at the same time. The diagnostic aspect uncovers abnormalities such as polyps, fibroids, adhesions, and congenital anomalies. The surgical aspect corrects these abnormalities and can improve fertility.
Intrauterine Pathologies and Infertility
Endometrial Polyps
Small, benign growths on the inner uterine wall can interfere with implantation or create an unfavorable environment for embryo development. Hysteroscopic polypectomy, the removal of polyps, has been shown to restore normal uterine function and improve fertility.
Uterine Fibroids (Myomas)
Submucosal fibroids distort the uterine cavity, decreasing the implantation rate and increasing the miscarriage rate. Hysteroscopic myomectomy is the preferred method to remove these fibroids and thus improve reproductive outcomes.
Intrauterine Adhesions (Asherman’s Syndrome)
Scar tissue in the uterus can block the uterine cavity, hinder implantation, and cause menstrual irregularities. Hysteroscopic adhesiolysis can restore the normal architecture of the uterine cavity, which is crucial for successful implantation and pregnancy.
Congenital Anomalies of the Uterus
Conditions such as a uterine septum, where a fibrous or muscular septum separates the uterine cavity, are associated with recurrent miscarriages. Hysteroscopic metroplasty, in which the septum is removed, significantly improves the chances of pregnancy.
Evidence from the Medical Literature
Numerous studies underline the positive effects of hysteroscopy on fertility:
- Endometrial Polyps: A systematic review by Kolibianakis et al. (2010) highlighted that hysteroscopic polypectomy in infertile women improves pregnancy rates in both natural and assisted reproductive scenarios, emphasizing the improved endometrial receptivity.
- Submucosal Fibroids: A landmark study by Pritts et al. (2009) showed higher conception rates in women who underwent hysteroscopic myomectomy compared to untreated women, concluding that removal of submucosal fibroids reduces mechanical obstruction and improves uterine receptivity.
- Intrauterine Adhesions: A retrospective analysis by Yu et al. (2008) found that hysteroscopic adhesiolysis significantly increased the pregnancy rate in women with Asherman’s syndrome. This underlines the importance of restoring the uterine cavity for successful embryo implantation.
- Septated Uterus: A meta-analysis by Homer et al. (2000) reported that hysteroscopic septal resection significantly improved reproductive outcomes.
Hysteroscopy in Assisted Reproductive Technology (ART)
Hysteroscopy plays a crucial role in optimizing the conditions for assisted reproductive technologies (ART) such as in vitro fertilization (IVF):
Pre-IVF Assessment
Routine hysteroscopy prior to IVF can detect and treat intrauterine abnormalities, increasing the chances of a successful pregnancy. A study by Rama Raju et al. (2006) showed that pregnancy rates improve after hysteroscopic intervention even in women with normal hysterosalpingography (HSG) findings.
Repeated Implantation Failure (RIF)
In women with RIF, hysteroscopy can diagnose and treat subtle intrauterine pathology not detected by other imaging modalities. Cenksoy et al. (2013) reported that hysteroscopic correction of these pathologies significantly improved subsequent IVF outcomes.
Safety and Efficacy
Hysteroscopy is generally considered safe and has a low complication rate. Common but rare complications include uterine perforation, infection, and bleeding. Advances in hysteroscopic technology and technique have minimized these risks and made hysteroscopy a reliable and effective procedure for improving fertility.
Future Directions
Ongoing research aims to refine hysteroscopic techniques and develop new instruments to further reduce complications and improve outcomes. The integration of hysteroscopy with advanced imaging technologies such as 3D ultrasound and MRI could improve the precision of both diagnostic and therapeutic procedures.
Conclusion
Hysteroscopy has proven to be a valuable tool for the diagnosis and treatment of intrauterine pathologies that contribute to infertility. Numerous studies show that hysteroscopy improves fertility by restoring the normal uterine environment, which is essential for implantation and pregnancy. As technology and techniques evolve, the effectiveness and safety of hysteroscopy is likely to continue to improve, further cementing its place in reproductive medicine.
The content has been created by Dr. Senai Aksoy and medically approved.
