What Exactly Are Uterine Polyps?
What Exactly Are Uterine Polyps?
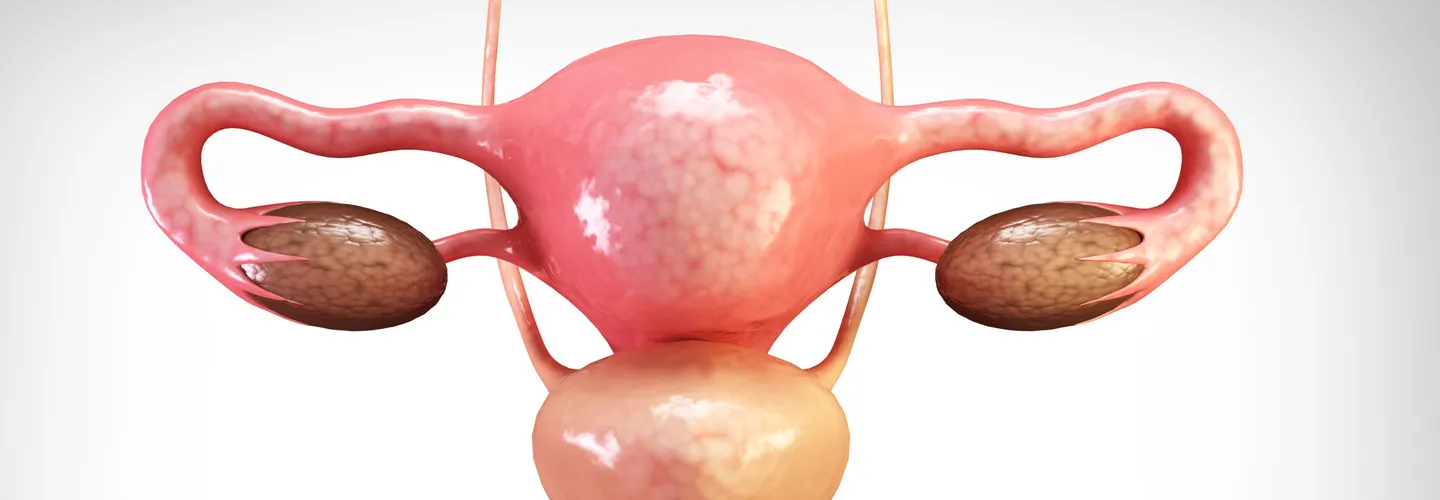
Uterine polyps, those little invaders in our uterus, are often whispered about, but today we shed some light on these mysterious little growths. Knowing about these unexpected visitors can be the first step to better health and a deeper understanding of our bodies. So are you ready for a quick lesson?
Simplified Medical Definition
Think of uterine polyps as tiny hanging gardens in the uterus. Except these benign growths are not flowers, they form when the tissue of the uterine lining, called the endometrium, starts to grow a little too enthusiastically. That’s certainly not the kind of gardening you’d want, is it?
Types to Get to Know
There are two main types of these little squatters: endometrial polyps, which settle in the lining of the uterus, and cervical polyps, which are located a little deeper in the cervical canal. Both types differ, but they have one thing in common: they should not be ignored under any circumstances.
Frequency of These Uninvited Guests
Contrary to what you might think, uterine polyps are not that rare. They are most common in menopausal women, but make no mistake, younger women are not spared either. Their prevalence is not to be taken lightly, so it’s important to talk openly about them and keep yourself well informed.
In summary, while uterine polyps may seem a little scary at first, once you learn more about their nature and how to treat them, they are much less frightening. Stay tuned as we delve deeper into the causes, symptoms, and possible treatments of these manageable but unwanted guests to our female health. Let’s uncomplicate it all together!
What Causes Uterine Polyps? A Story of Hormones and More
Dive into the fascinating world of hormones, where estrogens often play the leading role. These hormones, which are so important for our reproductive health, can sometimes become real double agents. A hormonal imbalance, which is often observed at the beginning of menopause, can lead to abnormal proliferation of the uterine lining. It’s as if these hormones turn into overzealous gardeners and turn our uterus into fertile ground for polyps. Not ideal, is it?
Risk Factors: A Slippery Slope
But that’s not all! Several other risk factors come into play. Obesity, for example, increases estrogen levels in the body, which also promotes the formation of polyps. Add to this high blood pressure and certain medications such as tamoxifen, which is used to treat breast cancer, and you have a cocktail that encourages the appearance of polyps. As you can see, it is a complex mixture of hormones, physical conditions, and environmental factors that prepares the ground for these invaders.
Menopause: A Crucial Period
The menopause is something of a major transition in the female body, and it plays a key role in the development of uterine polyps. The hormonal ballet is thrown out of balance, creating ideal conditions for these small growths to develop. However, it is important to know that polyps do not only occur at this stage of life. Even young women are not spared, which underlines how important it is to know your own body and stay informed.
A Complex Mixture of Causes
Ultimately, the causes of uterine polyps cannot be traced back to a single element. Rather, it is a potent cocktail of hormonal, individual, and physiological factors, such as those seen during menopause, that encourage their occurrence. A better understanding of this complexity can help you navigate the often alarming information and take a proactive approach to your reproductive health.
Symptoms of Uterine Polyps: Signals You Should Not Ignore
While uterine polyps are often inconspicuous, they can sometimes prove to be quite troublesome. Symptoms vary from woman to woman. Some women do not notice any signs at all, while others show clear signs.
- Abnormal Bleeding: This common symptom manifests as abnormally heavy menstruation or bleeding between cycles. Any deviation from your normal pattern requires attention. In addition, bleeding that occurs after menopause or after intercourse are important warning signs.
- Pain and Discomfort: Less common, but equally troubling, are pains or sensations of pressure in the lower abdomen that may indicate the presence of polyps. These sensations, sometimes accompanied by cramps, are worth a visit to the doctor.
- Fertility Problems: Polyps can present unexpected hurdles for women who wish to conceive. Sometimes they can be the cause of difficulty conceiving or recurrent miscarriages without any apparent symptoms.
It is important to remember that polyps can be present even without obvious symptoms. Therefore, regular visits to the gynecologist and appropriate follow-up examinations are crucial. These examinations allow for early detection of these unwanted guests and discussion of the best treatment options before symptoms become too bothersome or worsen.
How to Recognize Uterine Polyps? A Look at the Diagnostic Methods
The detection of uterine polyps is crucial for deciding on the best possible treatment. Fortunately, doctors have several highly effective diagnostic tools at their disposal. Here is an overview of the most important techniques for detecting these unwanted visitors in the uterus:
- Pelvic Ultrasound: This is often the first step. A pelvic ultrasound is a non-invasive method that uses sound waves to create images of the uterus. It is very useful for detecting abnormalities such as polyps, although it may require the assistance of other techniques to confirm the findings. Due to its simplicity and accessibility, it is a preferred tool for the initial examination.
- Hysterosonography: Hysterosonography involves the introduction of saline solution into the uterus to dilate the uterine cavity and provide a better view of the walls and possible polyps. This technique improves the clarity of the images compared to a standard pelvic ultrasound and therefore increases the accuracy of the diagnosis.
- Diagnostic Hysteroscopy: For a direct and precise view, nothing compares to hysteroscopy. This method uses a hysteroscope, a thin tube with a camera, to examine the inside of the uterus. It not only enables accurate detection of polyps, but also offers the possibility of a biopsy, i.e., the removal of a tissue sample for further analysis if necessary.
- Endometrial Biopsy: This technique, sometimes performed independently or during a hysteroscopy, involves taking a piece of tissue from the lining of the uterus and examining it under a microscope. It is particularly useful for determining whether polyps are precancerous or cancerous.
Each diagnostic method has its own strengths and limitations, but together they provide a comprehensive approach to accurately identify uterine polyps. It is crucial to proceed methodically and carefully, weighing up the pros and cons of each option to ensure a reliable diagnosis and choose a treatment tailored to each case.
Transparent communication between doctor and patient is essential to effectively navigate through these diagnostic options and ensure that each woman receives the individualized care she needs to manage her health as well and safely as possible.
Treatment Options for Uterine Polyps: Exploring the Options
There are very different approaches to treating uterine polyps depending on a woman’s individual needs. These include the condition of the symptoms, the size and number of polyps, and the woman’s fertility wishes. Tailored treatment is therefore crucial. Here are the main treatment methods available:
Hysteroscopic Polypectomy: The Preferred Technique
Hysteroscopic polypectomy is often preferred for the removal of polyps. In this procedure, which is performed under anesthesia, a hysteroscope is inserted into the uterus to remove the polyps directly. It is valued for its simplicity, short recovery time, and low risks, making it a common option.
Drug Treatment: A Gentler Alternative
Drug treatment is mainly considered when the polyps are small or when surgery is too risky. The medication used is often aimed at regulating hormone levels, which play a crucial role in the growth of polyps. However, it is important to emphasize that this type of treatment does not guarantee complete elimination of polyps and that regular monitoring is necessary to control the progression of polyps.
Hysterectomy: A Solution as a Last Resort
In the most complex cases, where polyps are numerous, recurrent, or associated with a risk of cancer, a hysterectomy — the surgical removal of the uterus — may be recommended. This is a major procedure that is usually reserved for situations where other treatments have failed or are not feasible, particularly in women who no longer wish to have children.
Specialized Consultation: A Must
Choosing the most appropriate treatment requires a thorough consultation with a specialist. It is crucial to understand all available options and choose a therapeutic path that takes into account all aspects of the patient’s health and wishes.
Impact of Uterine Polyps on Fertility: An Insurmountable Obstacle?
Uterine polyps can affect fertility in a number of ways, but fortunately, their effects are often reversible with the right treatment.
Fertility and Physical Obstacles
Polyps can physically block the path of the embryo or alter the hormonal environment of the uterus, making implantation difficult. Their presence can therefore be a serious obstacle for women who want to become pregnant.
Effectiveness of Polyp Treatment
The good news is that the treatment of polyps, particularly by hysteroscopy, can significantly improve fertility. Many women notice an improvement in their chances of conception after polyp removal.
Consultation and Aftercare: The Key to Success
For women facing polyps and wanting to get pregnant, it is important to see their doctor regularly to receive proper diagnosis and treatment. With today’s medical advances and proper follow-up care, uterine polyps should not be seen as an insurmountable obstacle on the road to motherhood.
In summary, while uterine polyps are a challenge, they are not necessarily a permanent obstacle to fertility. With accurate diagnosis and effective treatment, women can overcome this hurdle and achieve a successful pregnancy. The key is to take a proactive approach to managing their reproductive health.
The content has been created by Dr. Senai Aksoy and medically approved.
