Embryo 4AA, 3BB, 5BC. The Comprehensive Guide to Decoding Your Lab Report
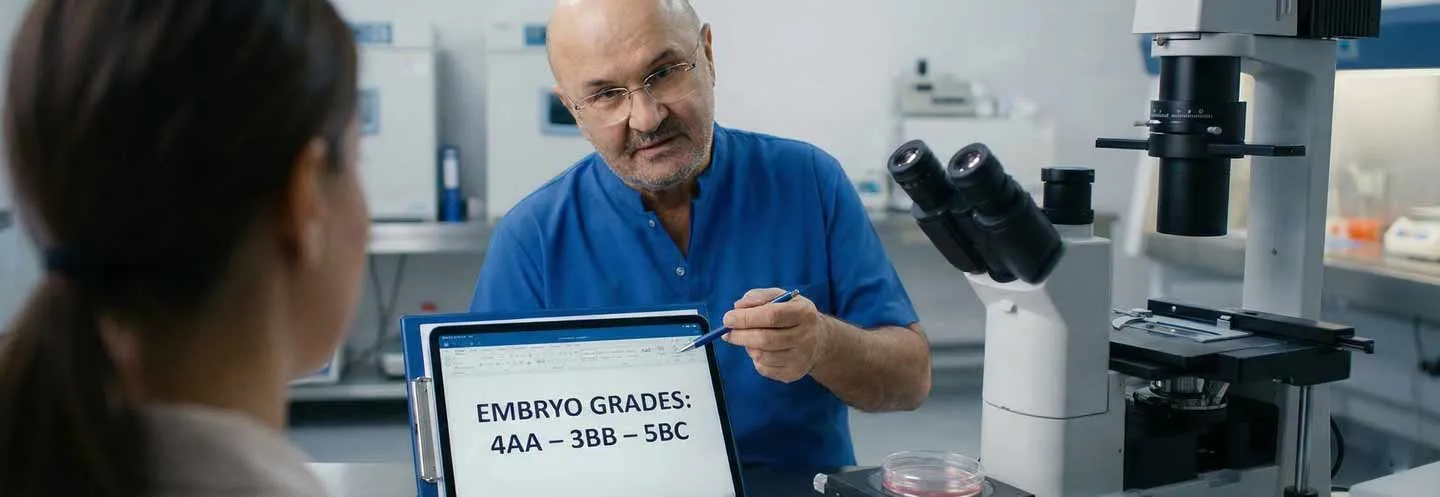
Embryo grading, like when you see a 4AA or 3BB on your chart, is how doctors sort embryos based on how they look under a microscope. Don’t think a good grade equals a guaranteed pregnancy, though. Docs check how far the blastocyst has come along (that’s the number, from 1 to 6), and they look at the inner cell mass (that’s the first letter, from A to C—it’ll be the baby) and the trophectoderm (second letter, also A to C—that becomes the placenta).
Sure, AA embryos have a better chance of implanting, but don’t count out those BB or BC embryos! They can still turn into healthy babies, especially if their genetics are normal. This is a simple explanation of what those codes mean, why looks aren’t everything, and how to think about picking the best embryo to transfer.
📌 What you will learn in this article
- Introduction: The Anxiety of the Report Card
- Basic Biology: From Egg Cell to Blastocyst (D0–D6)
- The Gardner System Decoded: The Da Vinci Code of IVF
- Dictionary of Grades: In-Depth Analysis (4AA, 3BB, 5BC…)
- The Istanbul Consensus: The New Scientific Reference
- The Crucial Importance of the Trophectoderm and Implantation
- Genetics Before Aesthetics: PGT-A and Mosaicism
- Time-Lapse and Morphokinetics: Film vs. Photo
- The Laboratory Environment and the Role of the Embryologist
- Transfer Strategies: Fresh vs. Frozen and Endometrial Preparation
- Influencing Factors: Age, Sperm, and Protocols
- FAQ: Direct Answers to Your Questions
1. Introduction: The Anxiety of the Report Card
Here in my clinic, where Europe shakes hands with Asia, I’ve assisted many couples in their dream of parenthood for three decades. The moment everyone anticipates, with bated breath, is when the embryo report appears. It reads like a stern verdict, packed with techy stuff and numbers.
I think of it like a heated soccer game, say Galatasaray versus Fenerbahçe. You’re in the stands, heart hammering, eager to see if your team—your embryos—scores. But instead of seeing the goal, you get a stats sheet: ball possession, pass accuracy, shots on target. That’s embryo grading for you—an analysis of your embryos’ state at a specific time. It doesn’t always tell you who will win, meaning have a healthy baby.
This is about making sense of that jargon. We’re turning those weird codes into something you can understand. We’ll look at why a 4AA is often seen as top-tier, but why a 3BB or even a 5BC can still pull off a surprise win.
Thematic Authority and Clinical Reality
Let’s be real, when it comes to reproductive medicine, it’s not black and white. It’s not just a simple score that gives you a yes or no answer. It’s all about the odds. So, just because an embryo is labeled as category C doesn’t mean it’s a lost cause. It’s still a chance, even if the odds are a bit different. What I’m here to do, and what this guide is all about, is to give you the knowledge to understand these results like you’re a pro. The goal is to keep you from freaking out, but to give you a clear idea of what’s going on.
2. Fundamental Biology: From Egg to Blastocyst (D0-D6)
To get scoring right, you gotta know what you’re looking at. Think of how embryos grow outside the body kind of like an wild obstacle course. Every step they nail is a win.
Day 0: Fertilization
It all begins when the sperm meets the egg. In our labs, we mostly go with ICSI (Intracytoplasmic Sperm Injection) if guys are having fertility problems, or if we want to up our odds of getting that egg fertilized.
-
How we do it: Our embryologist picks out the sperm that’s swimming the fastest and looks the best (sometimes using IMSI for a closer look) and then injects it right into a mature egg (MII).
-
What we look for: About 16 to 18 hours later, we take a peek to see if we spot two pronuclei (2PN). One carries Mom’s DNA, and the other, Dad’s. Spotting those means fertilization was a success.
Days 1 to 3: The Cleavage Stage
Okay, so now the cells are just splitting up. The little embryo isn’t getting any bigger right now, it’s just dividing into tinier bits inside its shell.
-
Day 2 (4 cells): Fingers crossed, we’ll see four cells that are all the same size and pretty clean.
-
Day 3 (8 cells): This is a big one! Before this point, the embryo has been living off mom’s leftovers from the egg. But once it hits eight cells, it has to turn on its own DNA (from the parents) to keep going. If an embryo isn’t so great, this is normally where it stops.
Day 4: The Morula and Compaction
So, first off, the cells get all cozy and stick real close. The lines between them start to fade. Then, the whole thing starts looking like a blackberry – that’s why they call it a morula.
- Heads up: This compaction thing is a big deal! It gets the cells chatting and ready to turn into different stuff. If the little embryo doesn’t do this by day four, chances are it won’t become a blastocyst later on.
Days 5 and 6: The Blastocyst
Okay, so here’s the gist of how it all goes down, at least from Gardner’s point of view:
-Cavitation: Think of it as tiny pumps (they’re actually called Na+/K+ ATPase) kicking into gear. They pump fluid into the embryo, which puffs up a bit and forms a little pocket, the blastocoel.
-Differentiation: This is where things get interesting. The cells start picking their jobs. Some are destined to become the actual baby (that’s the Inner Cell Mass, or ICM), and the rest will form the placenta (known as the Trophectoderm, or TE).
Dr. Aksoy’s take: Letting embryos grow to the blastocyst stage (around day 5) is a natural way to see which ones are strong. Not all fertilized embryos make it this far; about half drop off. It might sound intense, but it’s basically natural selection at work, helping pick the embryos with the highest chance of snuggling in and starting a pregnancy.
3. The Gardner System Decoded: The Da Vinci Code of IVF
Developed by David Gardner in the late 1990s, this system is the global standard. It breaks down the embryo into three distinct components. Understanding each component allows you to read your report like a professional. The Gardner system has been validated by numerous international studies and remains the gold standard for morphological evaluation of blastocysts.
1. The Number: Expansion (Volume)
Think of it like blowing up a balloon – this number (from 1 to 6) just shows how much it’s grown, not how good the balloon itself is.
| Grade | Stage | Clinical Description | Meaning for the Patient | |----------:|--------------------------|-------------------------------------------------------------------------------------------| ---------------------------------------------------------------------------------------------| | 1 | Early Blastocyst | Cavity occupies < 50% of the embryo volume | The embryo is just beginning to form its cavity. Often seen early in the morning on Day 5. | | 2 | Blastocyst | Cavity occupies > 50% of the embryo volume | Normal progression. | | 3 | Full Blastocyst | The cavity fills the entire embryo | The embryo has reached its “normal” size, but the shell is still thick. | | 4 | Expanded Blastocyst | The cavity is larger than the initial embryo; the shell is thinning | The ideal stage. The embryo pushes against the walls and is ready to emerge. | | 5 | Hatching | The embryo begins to emerge from its shell | Implantation process is imminent. Excellent sign of vitality. | | 6 | Hatched | The embryo has completely emerged from the shell | Very fragile due to lack of protection, but ready to implant immediately. |
2. The First Letter: Inner Cell Mass (ICM)
This is the group of cells that will become the fetus. It is obviously crucial. Morphometric studies have demonstrated the importance of the number and compactness of ICM cells in predicting the success of implantation.
-
A: It’s jam-packed with cells, a solid, round ball of them.
-
B: Here and there you’ll spot a cell, not as crowded together. Each one stands out on its own.
-
C: Barely any cells here. It’s tough to even figure out what it is.
3. The Second Letter: The Trophectoderm (TE)
Okay, so think of the placenta like this:
-
A: Imagine a super dense, thick layer – cells packed in tight, like a serious wall.
-
B: Then you’ve got a spot where the cells are a bit more spread out, not quite as crowded.
-
C: And finally, a delicate part with just a few big, oddly shaped cells. It is super easy to break.
4. Dictionary of Grades: In-Depth Analysis (4AA, 3BB, 5BC…)
This is where we answer the question: “Is my embryo good?” Let’s analyze the most common combinations with nuance and honesty. A recent multicenter study involving more than 10,000 transfers has provided a better understanding of the success rates associated with each grade.
Top Tier Grades: 4AA, 5AA, 6AA
-Analysis: These are the “top of the class.” They have maximum expansion and dense cell structures.
-Success Rates: Studies show clinical pregnancy rates of 60% to 70% (in women < 35 years old).
Just a heads-up: Even if an embryo looks great, like a top-notch 5AA, it doesn’t mean it’s problem-free. If you’re over 38, there’s still a chance it could have genetic issues. Think of it as a fancy car – you still need to pop the hood and check the engine, or in this case, the genetics.
“High Average” Grades: 3AA, 4AB, 4BA, 5AB
Almost perfect! One of the two setups (MCI or TE) got a B, but hey, that’s just one way to look at it. Big potential here. The odds of it working out are a lot like AA, usually hanging around 50-60%.
Dr. Aksoy mentioned that when picking between a 4AA and a 4AB embryo for transfer, they look pretty much the same to me. Both are great choices, in my opinion.
“Average” Grades: 3BB, 4BB, 5BB
What’s going on: So, this is where things are a little less than ideal, but hey, most IVF babies start here. The parts are all there, just not as many as we’d like.
The good news: It’s still pretty good! We’re looking at a 40-50% chance of pregnancy.
Bottom line: A BB embryo is totally okay. Don’t sweat it. In the real world, most embryos aren’t perfect AAs. A BB has got what it takes to make a healthy baby.
Low Average Grades: 3BC, 4CB, 5BC
Analysis: One of these isn’t quite as strong (C).
BC (MCI=B, TE=C): The future baby seems okay, but the placenta looks a bit fragile. There’s a chance it might not attach properly, which could lead to problems with implantation or an early miscarriage.
CB (MCI=C, TE=B): The placenta looks good, but the cell mass is a little weak. This can sometimes cause issues with the baby’s growth, but the embryo might be able to work around it.
Potential: Medium, around 25-35%.
Why keep them? Because a 30% chance is like one in three – that’s actually pretty good! If the embryo has normal genes, the odds get even better.
Poor Grades: CC
Analysis: Not a lot of cells here.
Potential: Pretty low, probably less than 15-20%. Lots of clinics don’t like freezing these kinds of embryos since they don’t thaw very well.
Exception: If this is the only embryo you’ve got during your fresh cycle, it’s still worth trying to transfer it. There have been babies born from these transfers.
5. The Istanbul Consensus: The New Scientific Reference
While the Gardner system is the most widely used clinically, the scientific community has sought to further standardize assessments. This is the objective of the Istanbul Consensus, developed by the ESHRE (European Society of Human Reproduction and Embryology) and Alpha Scientists in 2011, then updated in 2025.
Why a new standard?
The “A, B, C” rating system involves a degree of subjectivity. What is a ‘B’ in Istanbul may be an “A” in New York. The Istanbul Consensus aims to standardize these criteria so that global research is comparable.
Consensus Criteria
Basically, we can sort embryos into three groups based on how they look:
1- Good: These are the best ones, usually graded AA or AB/BA using the Gardner scale.
2- Average: These embryos get a BB grade.
3- Poor: These embryos are given a C grade.
The Concept of “Ranking” vs. “Grading”
Here’s the main difference between grading and ranking:
-Grading: This is just giving a score, like 4AA.
-Ranking: This is when we put embryos from the same group in order to decide which one to transfer first.
-How we do things: In my lab, we use Gardner grades to explain things to you. But we rank embryos like they say in the Istanbul consensus. So, if you have a 4AA and a 4BB, the 4AA goes first. And if you have two 4BBs, we check other things (how they grew, what they looked like at first) to see which one is the better choice.
6. The Crucial Importance of the Trophectoderm and Implantation
There is an ongoing debate among embryologists: What matters most? The baby’s grade (MCI) or the placenta’s grade (TE)? For a long time, MCI was thought to be king. After all, it’s the baby. But recent studies suggest that the Trophectoderm (the 2nd letter) may be the best predictor of pregnancy.
Why is TE so important?
-
Getting Started: The outer layer of cells (TE) has to get into the uterus wall. If this layer isn’t strong enough (grade C), the embryo won’t stick. If it doesn’t stick, you won’t get pregnant, even if the inner cell mass (ICM) looks great.
-
Making hCG: The outer layer cells make the pregnancy hormone hCG. It tells your body, I’m here, skip the period.
-
Miscarriage Risk: A weak outer layer means a higher chance of miscarriage in the first three months.
What to tell people: When picking between a 3AB embryo (inner cells=A, outer layer=B) and a 3BA embryo (inner cells=B, outer layer=A), many doctors suggest the 3BA embryo. They think a strong placenta is more important for the embryo to implant well.
7. Genetics before aesthetics: PGT-A and mosaicism
This could change medicine a lot. What we see isn’t everything since our genes really control things.
PGT-A (Preimplantation Genetic Testing for Aneuploidy)
This technique involves taking a few cells from the trophectoderm (biopsy) to analyze the number of chromosomes. Modern technologies use next-generation sequencing (NGS) for a complete analysis of all 24 chromosomes.
-
Euploid: 46 chromosomes (normal).
-
Aneuploid: Abnormal number (e.g., trisomy 21, monosomy). These embryos lead to implantation failure or miscarriage, or to congenital abnormalities.
The Golden Rule: Euploidy > Morphology
A 4CC euploid embryo is more likely to result in a baby than a 4AA aneuploid embryo. That is why, for patients over 38 years of age, or after repeated failures, I often recommend PGT-A. This allows us to avoid wasting time transferring embryos that are that are “beautiful” but genetically incompetent. Recent studies show that PGT-A can significantly reduce the miscarriage rate.
The Complex Case of “Mosaics”
Sometimes, the result comes back as “mosaic.” This means that the sample contains a mixture of normal and abnormal cells. Research on mosaicism has evolved considerably in recent years.
-
Low mosaicism (less than half abnormal): These embryos can fix themselves. The bad cells go to the placenta, so the baby grows from the good cells. You can transfer these, and they can become healthy babies.
-
High mosaicism (more than half abnormal): The odds of success aren’t as good, but sometimes it’s the only choice.
-
Making choices about this stuff is tricky and needs a long chat with a genetics expert.
8. Time-Lapse and Morphokinetics: Film vs. Photo
The usual (Gardner) way to check on embryos is static. You take them out of the incubator once a day to look at them. It’s kind of like trying to judge how good a marathon runner is by only seeing one photo of them at the end.
Time-Lapse Technology (Embryoscope)
In our laboratory, we use incubators equipped with cameras that take a photo every 10 minutes. This creates a film of the development, allowing us to analyze the morphokinetics (the timing of divisions). Modern time-lapse systems allow continuous monitoring without disrupting culture conditions.
Key Parameters (t2, t3, t5, cc2)
We keep a close watch on when things happen. Research suggests these things can help us figure out what’s coming next:
-
t2: This is when the first cell splits in two. If it happens too soon (before 8 p.m.) or too late, something’s not right.
-
cc2: How long the cell division lasts.
-
Direct Division: If a cell splits straight into three instead of two (1 - 3), that’s a really bad sign genetically. You won’t spot it just by looking unless you catch it at the exact moment.
With this information, algorithms (sometimes with the help of AI) can be used to give a viability score (e.g., KIDScore). This score complements the Gardner grade. A recent meta-analysis showed that the use of time-lapse with morphokinetic selection improves pregnancy and live birth rates.
9. The Laboratory Environment and the Role of the Embryologist
It’s easy to overlook this, but for about 5 to 6 days, the lab is like a womb for your embryos. Things such as air quality, temperature, and the culture they’re in really affect how well they do.
The Invisible Factors
-
Air quality (VOCs): Embryos don’t do well when exposed to things like perfumes or pollution. That’s why our labs are set up like clean rooms. They’re kept under pressure and have a really good filtration system.
-
Temperature: Even a tiny change in temperature can mess with how embryos grow. So, we use heated tables and incubators to keep the temperature steady.
-
Culture media: We use special culture media that copy the nutrients found in the fallopian tubes and uterus. This includes things like glucose, pyruvate, and amino acids.
The Human Factor
How an embryo is rated really comes down to the embryologist checking it. We have things in place to keep ratings consistent, but personal opinion always plays a part. So, a 3BB embryo here might be a 4BB somewhere else. Don’t focus too much on the exact grade. Think of it as one lab’s professional take.
10. Transfer Strategies: Fresh vs. Frozen and Endometrial Preparation
Having a good embryo is not enough. It must be placed in fertile ground.
Fresh Transfer
-What’s great: You don’t have to wait around – it all happens right away.
-What’s not so great: Your body still has those stimulation hormones hanging around. Also, the lining of your uterus might be ready too soon or just not at the same time as everything else. This can make it harder for the embryo to implant, even if it’s a healthy one.
Freeze-All and TEC
Okay, so here’s my take on how we handle things when women have a strong reaction to treatment, or when we use PGT-A testing:
-
How it goes: We freeze the embryos and give the body one cycle to get hormones back on track. Then, we gently get the uterus ready, either with hormones or by letting your natural cycle do its thing.
-
The upside: The uterus is ready when it needs to be. This usually works out better, and there’s no chance of overstimulating your ovaries.
-
Embryo quality – what’s the deal? Freezing methods these days are really good. Over 98% of embryos make it through. A good embryo stays good even after freezing. It might look a little different at first, but it bounces back quickly.
11. Influencing Factors: Age, Sperm, and Protocols
Why did you get 3BB and not 4AA?
Maternal Age and Ovarian Reserve
This is the dominant factor. The mitochondria (energy centers) of oocytes age. An “aged” oocyte has less energy to ensure cell division and blastocyst expansion. This is why grades tend to decline with age.
The Male Factor (Sperm)
People used to think sperm was just for getting someone pregnant. Turns out, that’s not the whole story. What the sperm contributes is important for starting genome activation on day 3. If the sperm’s DNA is in bad shape, it can mess up development on day 3, or you might end up with poor blastocyst formation.
The Stimulation Protocol
The drugs you pick (FSH, LH) and the treatment plan (antagonist, PPOS) can change how good your eggs are. If you get too much stimulation, you might end up with eggs that aren’t as good. I like to make a plan that fits each person, changing the amount of medicine to get good eggs instead of just a lot of them.
12. FAQ: Direct Answers to Your Questions
Here are the questions I hear every day in my office, answered without jargon.
Q1: “Is a 3BB embryo a ‘bad’ embryo? “
A: No, definitely not. B means Good. A 3BB embryo is a good, standard one. Most IVF pregnancies happen with embryos like this. The success rate is about 40-50%, which is great. Don’t worry that there’s no A.
Q2: “My embryo contracted after thawing. Is it dead?”
A: No. Think of a blastocyst as a water balloon. When we freeze it, we take some of the water out. After it thaws, it needs to absorb water again. It’s totally normal for it to look a bit wrinkled or smaller (grade 2 or 3) right after warming. But if it starts to expand again in the next few hours after that, it’s a really good sign that it made it!
Q3: “Why not transfer two average embryos (3BC) instead of one?”
A: Sure, it’s possible, but there are risks. If both embryos stick, a twin pregnancy can bring more problems, like early delivery or gestational diabetes. Also, some studies say that the womb might reject a good embryo because of the other one, but we’re not totally sure about that. Usually, we’d rather put in just one embryo—the one we think is most likely to work—especially if you’re younger or haven’t had many failed attempts.
Q4: “Can I improve the grade of my embryos for next time?”
A: We can’t alter our genes, but we can tweak how we live.
-
Lifestyle: Quitting smoking and keeping a healthy weight are very important.
-
Supplements: Coenzyme Q10 (Ubiquinol) might help the mitochondria in egg cells work better.
-
Procedure: The stimulation plan can be changed such as including LH or switching the trigger or using better sperm selection methods like Zymot or IMSI to help create higher quality blastocysts.
Q5: “What does ‘Assisted Hatching’ mean?”
A: Sometimes, especially after freezing, the embryo’s outer shell can be a bit too thick. When this happens, we use a laser to create a small opening in the shell. This helps the embryo hatch and attach to the uterus correctly, hopefully making it better. We often do this in my lab for frozen embryos or when the patient is older.
Conclusion: Beyond the Letters, the Promise of Life
So, keep in mind that your lab report is just a helpful tool, not a guarantee of success.
-
A 4AA is a really good start, but it doesn’t mean it will work.
-
A 3BB is a strong one that often does well.
-
A 5BC can even win sometimes, especially if it’s healthy(euploidy).
Fertility treatment involves both advanced tech and accepting that nature plays a big role. I’m here to use these scores to improve your odds each try, and we’ll adjust our plan if needed. You just need to stay hopeful and look after yourself. If you have this report, know that every embryo listed offers you a good shot at success. Trust us to pick the best one to transfer.
For more information on our website:
- IVF protocols and medications
- Fertilization: IVF and ICSI
- After the transfer: Complete guide to care and symptoms
Date of publication: December 19, 2025. This article was written for informational purposes by Dr. Senai Aksoy. Each patient is unique. The results of in vitro fertilization vary depending on many factors. Always consult a specialist for your personal situation.
© Dr. Senai Aksoy
The content has been created by Dr. Senai Aksoy and medically approved.

