The Role of Hysteroscopy in Female Infertility. An Evidence-Based Guide for Evaluation and Management

The Role of Hysteroscopy in the Evaluation and Management of Female Infertility: An Evidence-Based Clinical Report
Introduction: Why Hysteroscopy Matters More Than You Think
Let me be honest with you: as a clinician, there’s a moment I’ll never forget. Years ago, I met a couple who’d spent months—no, years—searching for answers about their infertility. Every test was “normal.” Every ultrasound, “unremarkable.” And then, with one simple office hysteroscopy, we found a small endometrial polyp hiding in plain sight—a polyp that none of the scans had picked up. A 15-minute procedure changed the trajectory of their journey. They called me six months later with good news.
If you’re reading this as a patient, you might feel overwhelmed by acronyms and options. If you’re a clinician, you’re probably weighing cost, risk, and evidence. Let’s cut through the noise together. This guide will walk you through how and why hysteroscopy has become a pivotal tool in evaluating and treating female infertility—and what that really means for your clinical choices or your personal fertility journey.
The Hysteroscopic Procedure: Principles and Practice
Hysteroscopy is a minimally invasive procedure where a thin, lighted telescope (the hysteroscope) is inserted through the vagina and cervix, allowing direct visualization—and sometimes immediate treatment—of the uterine cavity. Imagine being able to look inside the uterus, live, and address problems on the spot, often without any abdominal incisions. That’s the power of hysteroscopy.
Diagnostic vs. Operative Hysteroscopy: “See” vs. “See-and-Treat”
- Diagnostic hysteroscopy is all about observation. We use it to confirm suspected abnormalities, usually after a less invasive scan (like a sonogram or HSG) picks up something suspicious. You’re just looking—but that’s already a huge leap from traditional imaging.
- Operative hysteroscopy takes things a step further. Here’s where “see-and-treat” really shines. Say we spot a polyp or a small fibroid—using the same scope, we can often remove or correct the problem immediately, avoiding a second surgery and all the stress and logistics that come with it.
Takeaway: With miniaturized instruments and the right training, many interventions now happen right in the office—quicker, safer, and with minimal downtime.
Step-by-Step: What Actually Happens During Hysteroscopy?
- Timing matters: For women with regular cycles, the best time is just after menstruation, when the uterine lining is at its thinnest and visibility is best. Sometimes, we use medication to prep the cervix or optimize timing.
- Procedure: The patient lies comfortably (usually in the dorsal lithotomy position), the cervix is cleaned, and—if necessary—gently dilated. The hysteroscope is then advanced, and saline is used to expand the cavity for better visualization. Many clinics now use the “vaginoscopic approach”—inserting the scope without a speculum—which reduces discomfort.
- Examination: Every surface is inspected: the uterine fundus, anterior and posterior walls, lateral sides, and the tubal ostia. If a pathology is found, specialized instruments can be introduced to treat it immediately under direct vision.
Comfort and Anesthesia
One of the biggest misconceptions? That hysteroscopy is always painful or requires general anesthesia. The truth: modern diagnostic hysteroscopy, especially with small-diameter scopes, is often done with no anesthesia or just a little local numbing. Operative procedures may need more, but most women go home the same day. Pre-procedure pain relief and compassionate, clear explanation make all the difference.
What to Expect After the Procedure
Most patients experience mild cramping or spotting, similar to a light period, for a few days. If carbon dioxide was used for distension, you might feel some shoulder pain (don’t worry, it’s temporary!). For infection prevention, we recommend a week or two of pelvic rest (no intercourse, tampons, or swimming). Serious complications are rare, but it’s crucial to know warning signs like heavy bleeding or fever.
Hysteroscopy: The Gold Standard for Uterine Cavity Assessment
In fertility evaluation, what’s happening inside the uterus is crucial. Hysteroscopy offers the only way to actually see—and sometimes instantly fix—what’s wrong, rather than just guess based on shadows or indirect images.
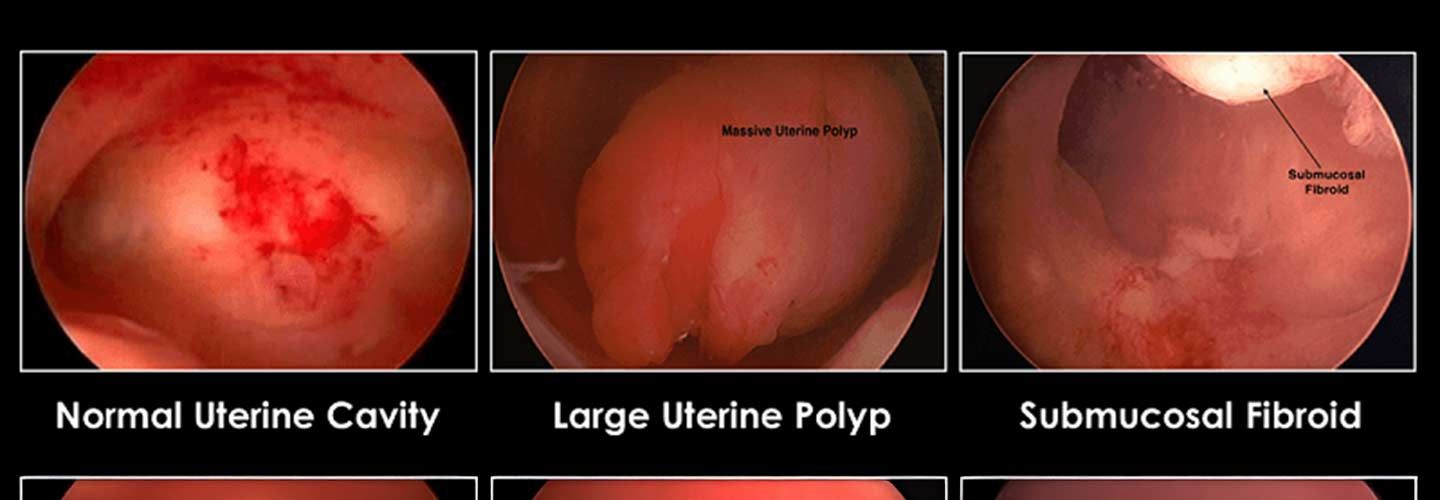
Spotting the Hidden Problems: What Can Hysteroscopy Diagnose?
- Endometrial Polyps: Benign growths that can sabotage implantation.
- Submucosal Fibroids: Fibroids that push into the cavity, distorting space for a potential embryo.
- Adhesions (Synechiae): Scar tissue that may block or distort the cavity (think Asherman’s syndrome).
- Congenital Anomalies: Like a uterine septum—often missed on regular imaging.
- Chronic Endometritis: Subtle inflammation sometimes only visible with direct hysteroscopic inspection.
Studies show that up to 50% of subfertile women have treatable abnormalities in the uterus—many completely silent and invisible on ultrasound.
Why Not Just Use Ultrasound or HSG?
Ultrasound and HSG (X-ray with contrast dye) are valuable, but have real limits. HSG, for example, has a high rate of “false positives”—finding “abnormalities” that aren’t really there, causing unnecessary anxiety and procedures. Saline infusion sonohysterography (SIS) is a much better initial screening tool than HSG, but even it misses subtle findings that hysteroscopy picks up. In some studies, nearly half of the abnormalities discovered by hysteroscopy were missed by other tests!
Table 1: At a Glance
| Method | What it’s best for | Weakness |
|---|---|---|
| Hysteroscopy | Direct vision, treatment | Most invasive |
| SIS | Great first screening | No treatment |
| HSG | Tube patency | Poor accuracy |
Operative Hysteroscopy: Not Just Diagnosis, But Cure
I’ll never forget the look of relief on patients’ faces when we could diagnose and treat a problem in the same session. The impact is real—not just emotionally, but biologically.
“See-and-Treat” Techniques That Change Outcomes
- Polypectomy: Remove polyps, often doubling pregnancy rates in IUI cycles.
- Myomectomy: Resection of submucosal fibroids, which can restore normal uterine shape.
- Metroplasty: Correction of septum, especially critical for recurrent miscarriages.
- Adhesiolysis: Removing scar tissue to open the cavity.
Not every abnormality needs to be treated, and not every intervention guarantees success. But for the right patient, the benefits are substantial and proven in trials—especially for polyps and septa.
The Real-World Evidence
The best outcomes are seen when we focus on lesions that clearly affect the cavity. Removing polyps and septa, in particular, is supported by strong evidence. For myomas and adhesions, the decision must be individualized.
Should Every Woman Undergoing IVF Have a Hysteroscopy?
Here’s where the debate gets hot. It’s tempting to do a hysteroscopy for every patient before IVF—after all, you want the best odds, right? But the science is nuanced.
- For asymptomatic women with normal initial imaging:
Routine hysteroscopy may increase clinical pregnancy rates but doesn’t reliably improve live birth rates. Leading guidelines (like NICE, ACOG, ASRM) do not recommend routine use. - For women with recurrent IVF failure or miscarriage:
The benefit is much clearer—hysteroscopy can reveal and fix problems that were missed, and this often makes the critical difference.
Bottom line:
Personalize the decision. For high-stakes cases, discuss the pros and cons openly.
Risks, Safety, and Future Trends: What Patients Deserve to Know
Hysteroscopy is one of the safest gynecological procedures, especially in experienced hands. Complications are rare (well below 1% for simple cases), but rise with complexity. Risks include perforation, bleeding, infection, or fluid overload—almost always manageable with prompt recognition.
The real revolution is in office-based, “see-and-treat” hysteroscopy. As instruments get smaller and more flexible, more patients can benefit with less downtime and cost.
Key Recommendations for Practice
- Don’t use hysteroscopy as the first test for every infertility case. Start with non-invasive imaging—SIS is the best first-line for the cavity.
- Move to hysteroscopy if imaging suggests a cavity abnormality, in recurrent implantation failure, or after recurrent miscarriage.
- For pre-IVF “screening,” reserve hysteroscopy for cases where the stakes are highest and discuss the limits of evidence honestly.
- Embrace office “see-and-treat” hysteroscopy for small, accessible lesions in appropriate patients.
- Counsel every patient clearly about the proven versus uncertain benefits, and tailor every decision to their unique clinical situation and goals.
FAQs: Honest Answers to Real Questions
Q: Will hysteroscopy improve my chances of pregnancy?
A: If you have a cavity abnormality (polyp, septum, etc.), yes—evidence shows significant improvement, especially after correction. For routine, “just in case” hysteroscopy, the benefit is less clear.
Q: Is it painful?
A: Most office hysteroscopies are described as mildly uncomfortable, not painful. Pre-procedure medication and a caring approach help immensely.
Q: How soon can I try to conceive after hysteroscopy?
A: For most simple procedures, you can try as soon as your next cycle—always confirm with your clinician.
Q: What are the main risks?
A: Major risks are rare. Most women have mild cramping and light bleeding. Severe complications are very uncommon when performed by experienced clinicians.
Q: Should I have hysteroscopy before my IVF cycle?
A: If you have risk factors or a history of failed cycles, discuss it with your doctor. Otherwise, current guidelines don’t recommend routine use.
Conclusion: Key Takeaways and Next Steps
- Hysteroscopy is the gold standard for seeing—and treating—problems in the uterine cavity.
- Correcting the right abnormalities can meaningfully improve reproductive outcomes.
- Routine use in all IVF cycles isn’t justified by current evidence; individualize every decision.
- Safety and comfort have improved dramatically with modern, office-based “see-and-treat” models.
- Always seek care from experienced providers, and don’t hesitate to ask all your questions—your voice matters.
Have you had a hysteroscopy, or are you considering one? What’s your biggest question or fear? Let’s open the conversation—share your experience or ask below!
Internal Links
External Link (high authority)
The content has been created by Dr. Senai Aksoy and medically approved.
